history of multiple sclerosis
 History of Multiple Sclerosis – MSAA
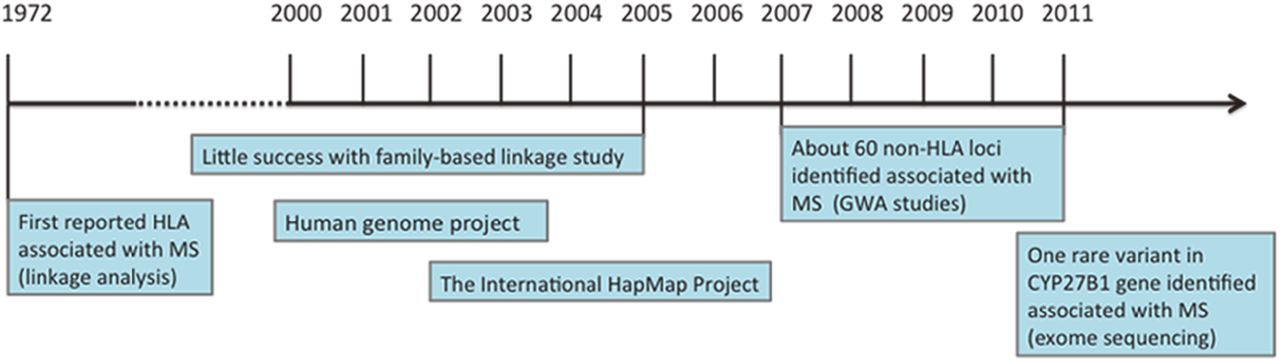
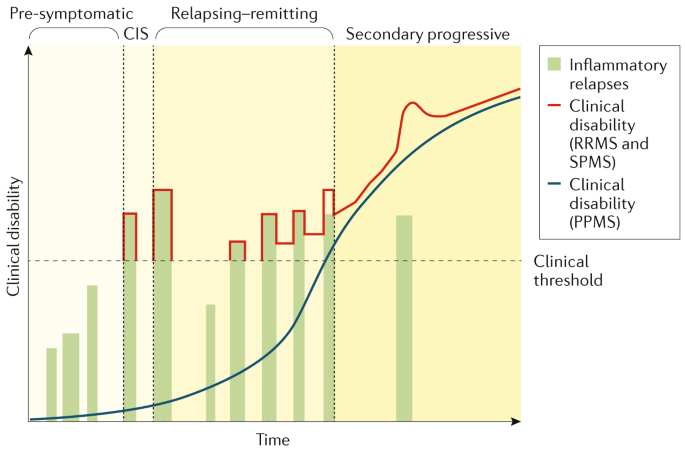
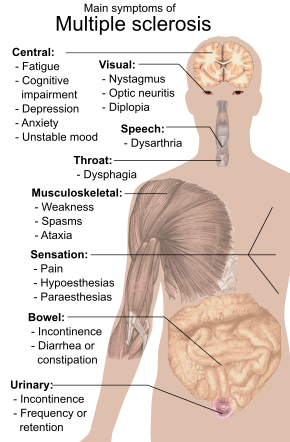
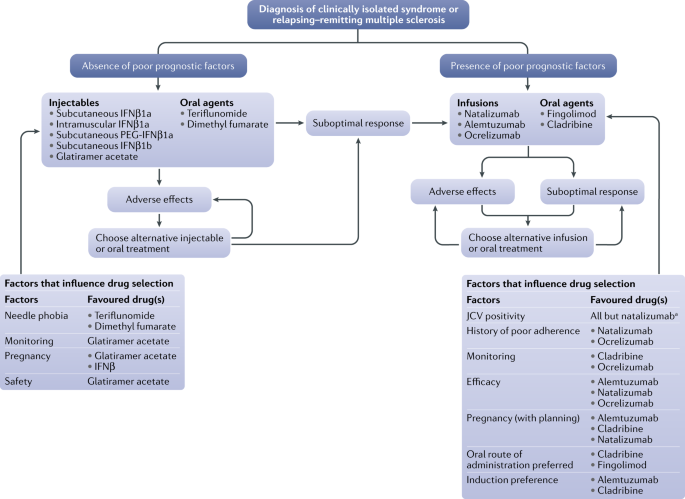
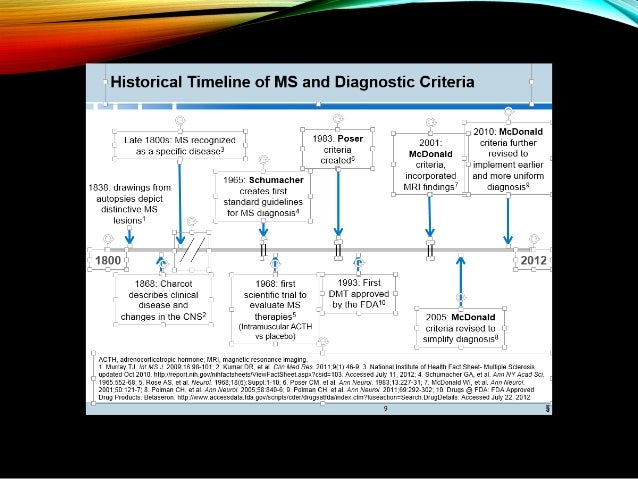
History of Multiple Sclerosis – MSAAMultiple sclerosis Multiple sclerosis Other namesDisseminate encephalomitis, disseminate-woven sclerosis shows several in the area of a demyelinated lesion caused by the EM. SymptomsDual vision, in one eye, muscle weakness, problems with , problems with coordination habitual inauguration Age 20–50DurationLong termCausesUnknown Based on symptoms and medical tests TreatmentMedications, physical therapyPrognosis5-10 shorter years Frequency2 million (2015)Muertes18,900 (2015)Multiple sclerosis (MS), also known as encephalomitis disse This damage disrupts the ability of parts of the nervous system to , leading to a range of physical, , and sometimes psychiatric problems. Specific symptoms may include , in one eye, muscle weakness and problems with or coordination. MS takes several forms, with new symptoms or occurs in isolated attacks (relapse forms) or accumulate over time (progressive forms). Among the attacks, the symptoms can disappear completely; however, permanent neurological problems often remain, especially as the disease progresses. Multiple sclerosisMSencephalomilitis disseminate Although the cause is unclear, the underlying mechanism is believed to be or fails of the producing cells. The causes proposed for this include and the environmental factors that are triggered by a . MS is usually diagnosed based on signs and symptoms of presentation and the results of medical support tests. There is no known cure for multiple sclerosis. Treatments try to improve function after attack and prevent new attacks. Medicines used to treat MS, although modestly effective, may have side effects and be poorly tolerated. can help with people's ability to work. Many people seek, despite the lack of evidence of benefit. The long-term result is difficult to predict; good results are more often seen in women, those who develop early disease in life, those who have a relapse course, and those who initially experienced few attacks. is on average five to ten years lower than that of the unaffected population. Multiple sclerosis is the most common one that affects . In 2015, around 2.3 million people were affected globally, with rates that vary widely in different regions and between different populations. In that year, about 18,900 people died of MS, of 12,000 in 1990. The disease usually begins between the ages of twenty and fifty years and is twice more common in women than in men. MS was first described in 1868 by French neurologist. The multiple name refers to the numerous (or scleras – essentially plates or lesions) that develop in the brain and spinal cord. Several new treatments and diagnostic methods are being developed. IndicesSigns and symptoms[] A person with MS may have almost any neurological symptoms or sign, with visual, motorized and sensory problems being the most common. Specific symptoms are determined by the locations of the lesions within the nervous system, and may include or such as tingling, nails and needles or numbness, muscle weakness, , , , , , or difficulty moving; difficulties with coordination and balance (); or , visual problems (, or ), or , and difficulties of bladder and intestine (such as ), among others. Difficulties of thought and emotional problems as well as common. , a worsening of symptoms due to exposure to higher temperatures than usual, and , an electrical sensation that runs through the back when the neck is folded, are particularly MS characteristics. The main measure of disability and gravity is (EDSS), with other measures such as the increasingly used being in the investigation. EDSS is also correlated with drops in people with MS. Although it is a popular measure, EDSS has been criticized for some of its limitations, such as relying too much on walking. The condition begins in 85% of cases like a (CIS) for several days with 45% having motorized or sensory problems, 20% having , and 10% having symptoms related to dysfunction, while the remaining 25% has more than one of the previous difficulties. The course of the symptoms occurs in two main patterns initially: either as episodes of sudden deterioration that last a few days to months (called, exacerbations, outbreaks, attacks or outbreaks) followed by improvement (85% of cases) or as a gradual worsening with time without recovery (10-15% of cases). A combination of these two patterns can also occur or people can start in a relapse and remission course that then becomes progressive later. Relapses are generally not predictable, they occur without warning. The exacerbations rarely occur more frequently than twice a year. Some relapses, however, are preceded by common triggers and occur more often during spring and summer. Similarly, viral infections such as , , or increase your risk. It can also trigger an attack. Women with MS experience less relapse; however, during the first few months after the risk is given, it increases. In general, pregnancy does not seem to influence long-term disability. Many events have been found to not affect relapse rates including , , physical trauma, and . Causes[] The cause of the EM is unknown; however, it is believed to occur as a result of some combination of genetic and environmental factors such as infectious agents. The theories try to combine data in probable explanations, but none has proved to be definitive. While there are several environmental risk factors and although some are partially modifiable, further research is needed to determine whether their elimination can prevent MS. Geography[] MS is more common in people who live farther from , although there are exceptions. These exceptions include ethnic groups that are at low risk away from the equator such as the , , Canadian , New Zealand , and Canada's , as well as groups that have a relatively high risk near the equator as , interior , , and . The cause of this geographical pattern is not clear. While the north-south incidence gradient is declining, since 2010 it is still present. MS is more common in regions with populations in northern Europe and geographical variation can simply reflect the global distribution of these high-risk populations. The decrease in sunlight exposure that has led to a decrease in production has also been presented as an explanation. A relationship between the birth season and the EM supports this idea, with fewer people born in the northern hemisphere in November compared to May being affected later in life. Environmental factors can play a role during childhood, with several studies finding that people moving to a different region of the world before the age of 15 acquire the risk of the new region to the EM. However, if migration takes place after the age of 15, the person maintains the risk of his or her country of origin. There are some evidence that the effect of the move can still be applied to people over 15 years of age. Genetics[]MS is not considered a disease; however, several have been shown to have increased risk. Some of these genes seem to have higher levels of expression in microglyal cells than expected by chance. The probability of developing the disease is greater in the relatives of an affected person, with a higher risk among the most closely related. Both are affected around 30% of the time, while about 5% for non-identical twins and 2.5% of the brothers are affected with a smaller percentage of half brothers. If both parents are affected by the risk in their children it is 10 times that of the general population. MS is also more common in some ethnic groups than others. Specifics that have been linked to the EM include differences in the system (HLA) — a group of genes in which it serves as the (MHC). These differences in the HLA region have been characterized by susceptibility since the 1980s, and this same region has also been involved in the development of other autoimmune diseases such as and . The most consistent finding is the association between multiple sclerosis and MHC defined as and . Other loci have shown a protective effect, like and *11. In general, it has been estimated that HLA differences represent between 20% and 60% of the . Modern genetic methods () have revealed at least twelve more genes outside HLA that modestly increase the probability of MS. Infectious agents[]Many have been proposed as MS triggers, but none have been confirmed. Moving to an early age from one place in the world to another alters the subsequent risk of a MS person. An explanation for this might be that some type of infection, produced by a generalized microbe instead of a rare one, is related to the disease. The proposed mechanisms include the prevalence hypothesis and the hypothesis. Hygiene hypothesis proposes that exposure to certain early infectious agents in life is protective, disease is a response to a late encounter with such agents. Prevalence hypothesis proposes that the disease is due to a more common infectious agent in regions where the EM is common and where, in most individuals, it causes a continuous infection without symptoms. Only in a few cases and after many years causes demystification. The hygiene hypothesis has received more support than the prevalence hypothesis. The evidence of a virus as a cause includes the presence of in the brain and most people with MS, the association of several viruses with human demiseation, and the appearance of demysilation in animals caused by some viral infections. are a candidate group of viruses. Individuals who have never been infected with have a reduced risk of getting MS, while those infected as young adults have a higher risk than those who have had it at a younger age. Although some consider this to be against the hypothesis of hygiene, since the uninfected have probably experienced more hygienic upbringing, others believe that there is no contradiction, since it is a first encounter with the relatively late causative virus in life that is the trigger of the disease. Other diseases that may be related include , and . Others [] may be an independent risk factor for MS. may be a risk factor, although the evidence supporting this is weak. The association has been evaluated with occupational exhibitions and, above all, no clear conclusions have been reached. were studied as causal factors; however, most studies do not show association. Other possible risk factors such as intake and intake have been examined; however, the evidence about their relationship with the disease is "spread and unpersuasive". occurs less than expected and lower levels have been found in people with MS. This has led to the theory that uric acid is protective, although its exact importance remains unknown. Pathophysiology[p] ] The three main characteristics of the EM are the formation of lesions in the (also called plates), inflammation and destruction of neurons. These characteristics interact in a complex and still uninformed way to produce the breakdown of the nervous tissue and in turn the signs and symptoms of the disease. both are believed to harm the repair of myelin and exacerbate inflammation. It is believed that the EM is a disorder that develops from an interaction of the individual's genetics and so far unidentified environmental causes. The damage is believed to be caused, at least in part, by an attack on the nervous system by a person's own immune system. Lesions[]The name of multiple sclerosis refers to scars (sclerae – best known as plates or lesions) that form in the nervous system. These lesions most commonly affect the pathways of matter, , , and , or of white matter near the side . The function of white matter cells is to carry signals between areas, where the processing is done, and the rest of the body. She's rarely involved. To be specific, MS involves loss of , the cells responsible for creating and maintaining a fat layer — known as the pod — that helps the neurons carry (possibilities of action). This leads to a loss of myelin or thin and, as the disease progresses, the breakdown of neurons. When you lose myelin, a neuron can no longer drive electrical signals effectively. A process of repair, called, takes place in early stages of the disease, but oligodendrocytes are unable to completely rebuild the myelin pod of the cell. Repeated attacks lead to successively less effective remissions, until a plate similar to the scar is built around the damaged axes. These scars are the origin of symptoms and during an attack (RM) often shows more than ten new plates. This might indicate that there are a number of injuries under which the brain is capable of repairing without producing significant consequences. Another process of creating injuries is abnormal due to the destruction of nearby neurons. Several have been described. Inflammation[] Apart from demysilation, the other sign of the disease is . Fixing with an explanation, the inflammatory process is caused by, a species that plays an important role in the defenses of the body. T cells gain entry into the brain through interruptions in the . T cells recognize myelin as a foreigner and attack it, explaining why these cells are also called "self-reactive reports". The attack on myelin begins inflammatory processes, which triggers other immune cells and the release of soluble factors such as and . A new breakdown of the blood-brain barrier, in turn, causes a number of other harmful effects such as , activation of , and more activation of cytokines and other destructive proteins. Inflammation can potentially reduce the transmission of information between neurons in at least three ways. The released soluble factors could stop neurotransmission by intact neurons. These factors may lead to or improve myelin loss, or may cause axon to completely decompose. Blood Brain Barrier[]The (BBB) is a part of the system that prevents T-cell entry into the central nervous system. It can be permeable to these types of secondary cells to an infection by a virus or bacteria. After repairing, typically once the infection has been cleared, T cells can stay trapped inside the brain. it cannot cross a normal BBB and therefore the increased RRM of gadolinium is used to show the BBB breakdown. Diagnosis[p] ]This article must be updated. Please update this article to reflect recent developments or information recently available. (July 2020)updatedMulti-sclerosis is usually diagnosed based on signs and symptoms of presentation, in combination with support tests and laboratory. It may be difficult to confirm, especially early, as signs and symptoms may be similar to those of other medical problems. The , which focuses on clinical, laboratory and radiological evidence of lesions at different times and in different areas, is the most used diagnostic method with it and be of greater historical importance. Clinical data alone can be sufficient for a diagnosis of MS if an individual has had separate episodes of neurological symptoms characteristic of the disease. In those seeking medical care after a single attack, other diagnostic tests are needed. The most used diagnostic tools are , the analysis of the cerebrospinal fluid and . of the brain and spinal column can show areas of demitalization (lesions or plates). can be given as one to highlight active plates and, by elimination, demonstrate the existence of historical lesions not associated with symptoms at the time of evaluation. The analysis of cerebrospinal fluid obtained from one can provide chronic evidence in the central nervous system. The cerebrospinal fluid is tested for IgG in , which are inflammation markers found in 75-85% of people with MS. The nervous system in MS can less actively respond to the stimulation of and due to the demystification of such paths[] i.e. less than a normal of 70mA.[][] These brain responses can be examined using - and sensory-. Although the above criteria allow for a non-invasive diagnosis, and although some claim that the only definitive test is one or where typical EM lesions are detected, there is currently no single test (including biopsy) that can provide a definitive diagnosis of this disease. Types and variants have been described[]Several (types commonly referred to), or progression patterns. Phenotypes use the past course of the disease in an attempt to predict the future course. They are important not only for prognosis, but also for treatment decisions. Currently, the United States and the , describes four types of MS (revised in 2013): MS recapitulation is characterized by unpredictable relapses followed from months to years of relative tranquility () without new signs of disease activity. The deficiencies that occur during the attacks can resolve or leave, the latter in about 40% of the attacks and be more common the longer the disease has. This describes the initial course of 80% of individuals with MS. Relapse subtype usually begins with isolated clinical syndrome (CIS). In the CIS, a person has a suggestive attack on demystification, but does not meet the criteria for multiple sclerosis. 30 to 70% of people who experience CIS, later develop the EM. Primary progressive MS occurs in approximately 10-20% of individuals, without referral after initial symptoms. It is characterized by progression of disability from the outset, without, or only occasional and minor, referrals and improvements. The usual starting age for the progressive primary subtype is later than the relapse subtype. It is similar to the age that the progressive secondary usually begins in relapse-remitting MS, about 40 years old. The secondary progressive MS occurs in about 65% of those who present an initial relapse, which eventually have a progressive neurological decrease between acute attacks without any defined period of remission. Occasional relapses and minor remissions may appear. The most common duration between the beginning of the disease and the conversion of relapse-remitting to the secondary progressive EM is 19 years. Multiple sclerosis behaves differently in children, taking more time to achieve the progressive stage. However, they still reach an average age less than adults. Special courses[] Regardless of the types published by MS associations, regulators such as FDA usually consider special courses, trying to reflect some clinical trial results in their approval documents. Some examples could be "Highly active SMS" (HAMS), "active secondary SMS" (similar to the old progressive relapse) and "PPMS progressing quickly." Moreover, when deficits are always solved between attacks, this is sometimes called benign MS, although people will still accumulate some degree of long-term disability. On the other hand, the term is used to describe people with MS who have reached a significant level of disability in a short period. As of June 2020 an international panel has published a standardized definition for the HAMS course Variants[] The MS atypic has been described; these include , , and . There is debate about whether they are MS variants or different diseases. Some diseases previously considered variants of MS as they are now considered outside the MS spectrum. Management[] Although there is no cure known for multiple sclerosis, several therapies have proven to be useful. The main objectives of therapy are re-operating after an attack, avoiding new attacks and avoiding disability. The initiation of medicines is usually recommended in people after the first attack when more than two lesions are observed in the MRI. As with any medical treatment, the medications used in the management of the MS have several. they are persecuted by some people, despite the shortage of supporting evidence. Acute Attacks[]During symptomatic attacks, the administration of high doses of , such as , is the usual therapy, with oral corticosteroids appear to have a similar safety and efficacy profile. Although it is short-term effective to relieve symptoms, corticosteroid treatments do not seem to have a significant impact on long-term recovery. Long-term benefit is not clear in optical neuritis in 2020. The consequences of serious attacks that do not respond to corticosteroids could be treated by . Treatments that modify diseases[]Recating the remission of multiple sclerosis[] Starting in 2020, regulatory agencies approve multiple medicines that modify diseases to relapse multiple sclerosis (RRMS). They're, , , , , , , , , , , , , , , and . Its cost effectiveness since 2012 is unclear. In March 2017, the FDA approved , an anti- , as treatment for RRMS, with requirements for several clinical trials. RRMS are modestly effective in reducing the number of attacks. Interferons and glatiramer acetate are first-line treatments and are approximately equivalent, reducing relapse by about 30%. Long-term therapy early started is safe and improves results. Natalizumab reduces the relapse rate more than frontline agents; however, due to adverse effects problems it is a second line agent reserved for those who do not respond to other treatments or with serious illnesses. Mitoxantrone, whose use is limited by serious adverse effects, is a third-line option for those who do not respond to other medications. The treatment of isolated clinical syndrome (CIS) decreases the likelihood of progressing to clinical MS. It has been estimated that the effectiveness of interferons and glatiramer acetate in children is approximately equivalent to that of adults. The role of some newer agents such as fingolimod, teriflunomide and dimethyl Smokingate is still not completely clear. It is difficult to reach firm conclusions about the best treatment, especially in relation to the long-term benefit and safety of early treatment, given the lack of studies that directly compare diseases by modifying therapies or the long-term monitoring of patient outcomes. Since 2017, it was widely used outside the label to treat RRMS. There is a lack of high-quality randomized control tests that examine rituximab versus placebo or other therapies that modify the disease, and as such the benefits of rituximab to relapse the multiple sclerosis that is sent are still not included. The relative effectiveness of the different treatments is not clear, as most have been compared only to placebo or with a small number of other therapies. Direct comparisons of similar effects or only small differences of effects on relapse rate, disease progression and measures. Alemtuzumab, natalizumab and fingolimod may be more effective than other medications to reduce short-term relapses in people with RRMS. and () may reduce relapses compared to placebo and () while (), and may also prevent relapses. It is unclear whether there is evidence of relative effectiveness in reducing progression of disability. All medicines are associated with adverse effects that may influence your risk to benefit profiles. Progressive multiple sclerosis[]From 2013, the 9 review found no evidence that any being effective in preventing the progression of disability in people with progressive MS. Since 2017, rituximab has been widely used outside the label to treat progressive primary EM. In March 2017 the FDA approved ocrelizumab as a treatment for progressive primary EM, the first drug to obtain that approval, with requirements for several clinical trials. Since 2011, only one medication, mitoxantrone, had been approved for progressive secondary MS. In this population, the provisional tests support the mitoxantrona by moderately slowing down the evolution of the disease and decreasing relapse rates for two years. In 2017, it was approved in the United States for the treatment of progressive primary multiple sclerosis in adults. It is also used for the treatment of the relapse forms of multiple sclerosis, to include isolated clinical syndrome, relapse-remittent disease and active secondary progressive disease in adults. In 2019, and were approved in the United States for the treatment of multiple secondary sclerosis. Adverse effects[ ] Disease modification treatments have several adverse effects. One of the most common is irritation at the injection site for glatiramer acetate and interferons (up to 90% with subcutaneous injections and 33% with intramuscular injections). Over time, you can develop a visible denture on the injection site, due to the local destruction of fat tissues known as . Interferons can produce; some people who take a glatiramer experience experience experience experience experience experience a post-injection reaction with flu, chest stiffness, heart palpitations and anxiety, which usually last less than thirty minutes. More dangerous but much less common are interferons (12%), and (0.8%) of mitoxantrone, and occur with natalizumab (acting in 1 in 600 people treated). Fingolimod can give rise to and , , elevated liver enzymes or . Provisional evidence supports short-term security of teriflunomide, with common side effects, including: headaches, fatigue, nausea, hair loss and member pain. There have also been reports of liver and PML insufficiency with its use and is . The most common side effects of dimethyl smokingate are gastrointestinal problems. While dimethyl smoking may lead to one, cases of opportunistic infections were not reported during trials. Associated symptoms[]Both medicines and have been shown to improve some symptoms, although none changes the course of the disease. Some symptoms have a good response to medication, such as bladder spasticity, while others are unchanged. The equipment as for mobility aids or aids can be useful to improve the functional state. An approach is important to improve quality of life; however, it is difficult to specify a 'basic team' as many health services can be needed at different points in time. Multidisciplinary rehabilitation programmes increase the activity and participation of people with MS but do not influence the level of deterioration. Studies investigating the provision of information in support of patient understanding and participation suggest that, while interventions (written information, decision-making aid, training, educational programs) may increase knowledge, evidence of an effect on decision-making and quality of life is mixed and of low certainty. There is limited evidence for the overall effectiveness of individual therapeutic disciplines, although there is good evidence that specific approaches, such as exercise and psychological therapies are effective. Cognitive formation, alone or combined with other neuropsychological interventions, can show positive effects for memory and attention, although firm conclusions are not currently possible given small sample numbers, variable methodology, interventions and results measurements. The effectiveness of standard care is uncertain, due to lack of evidence. The effectiveness of interventions, including exercise, specifically for the prevention of falls in people with EM is uncertain, while there are some evidence of an effect on the function of balance and mobility. has proven to be moderately effective in reducing MS fatigue. Tests for the effectiveness of non-pharmacologic interventions for chronic pain are not sufficient to recommend such interventions alone, however their use in combination with medications may be reasonable. Alternative treatments[]More than 50% of people with MS can use, although the percentages vary depending on how alternative medicine is defined. As for the characteristics of users, they are more often women, have had MS for longer, tend to be more disabled and have lower levels of satisfaction with conventional medical care. In most cases, evidence of the effectiveness of these treatments is weak or absent. Untested benefit treatments used by people with MS include dietary supplements and regimens, vitamin D, such as , (including ), , , , , , , , and . Tests suggest that supplementation of vitamin D, regardless of form and dose, does not provide any benefit for people with MS; this includes measures such as relapse recurrence, disability and resonance lesions, while not being treated in the same way. High-dose biotin (300 mg/day = 10,000 times the right intake) has been studied clinically for the treatment of multiple sclerosis. The hypothesis is that biotin can promote the remylation of the nerve cell pod, slowing or even reversing neurodegeneration. The proposed mechanisms are that acetyl-coA carboxylase active biotin, which is a key rate limitation enzyme during myelin synthesis and reducing axonal hypoxia by means of improved energy production. Two reviews reported no benefits, and some evidence for increased disease activity and higher risk of relapse. Prognosis[] The expected future course of the disease depends on the subtype of the disease; the sex, age and initial symptoms of the individual; and the degree of the person has. Women's sex, relapsed subtype, optical neuritis or sensory symptoms at first, few attacks in the early years and especially early age at first, are associated with a better course. Average life expectancy is 30 years since the beginning of the disease, which is 5 to 10 years less than that of unaffected people. Almost 40% of people with MS reach the seventh decade of life. However, two thirds of deaths are directly related to the consequences of the disease. is more common, while infections and other complications are especially dangerous for the most disabled. Although most people lose the ability to walk before death, 90% are able to walk independently 10 years from the beginning, and 75% to 15 years. [] Epidemiology[p] ]This article needs to be updated. Please update this article to reflect recent developments or information recently available. (September 2020) MS is the most common autoimmune disorder of the . Since 2010, the number of people with MS was 2 to 2.5 million (approximately 30 per 100,000) worldwide, with rates that vary widely in different regions. It is estimated that 18,000 deaths occurred that year. In Africa the rates are below 0.5 per 100,000, while they are 2.8 per 100,000 in South-East Asia, 8.3 per 100,000 in America and 80 per 100,000 in Europe. Rates over 200 per 100,000 inhabitants in certain populations of European descent in the North. The number of new cases that take place per year is approximately 2.5 per 100,000. MS rates seem to be increasing; this, however, can be explained simply by better diagnosis. Studies on population and geographical patterns have been common and have led to a series of theories on the cause. MS usually appears in adults in the late twenties or early 1930s, but it can rarely start in childhood and after 50 years. The progressive primary subtype is more common in the people of its fifties. Similar to many autoimmune disorders, the disease is more common in women, and the trend may be increasing. Since 2008, around the world is approximately twice as common in women as in men. In children, it is even more common in women than in men, while in the elderly of fifty, it affects almost equal men and women. History[]Medical discovery[] (1793-1857), British professor of , and (1791-1873), French professor of pathological anatomy, described and illustrated many of the clinical details of the disease, but did not identify it as a separate disease. Specifically, Carswell described the lesions he found as "a remarkable spinal cord injury accompanied by atrophy." Under the microscope, the Swiss pathologist (1836-1908) pointed out in 1863 that the lesions associated with inflammation were distributed around the blood vessels. The Frenchman (1825-1893) was the first person to recognize multiple sclerosis as a different disease in 1868. Adding previous reports and adding his own clinical and pathological observations, Charcot called the sclera of the disease on plaques. History of diagnosis[] The first attempt to establish a set of diagnostic criteria was also due to Charcot in 1868. He published what is now known as the "Triada de Charcot", consisting of , , and (spoke in Canning) Charcot also observed cognitive changes, describing his patients as having a "marked memory disease" and "conceptions that slowly formed." The diagnosis was based on the triad of Charcot and clinical observation until the first attempt was made to standardize criteria in 1965 by introducing some fundamental requirements: Dissemination of the lesions in time (DIT) and space (DIS), and that "signs and symptoms cannot be better explained by another disease process." Both requirements were subsequently inherited by and , whose 2010 version is currently in use. During the twentieth century, theories on cause and pathogenesis were developed and effective treatments began to appear in the 1990s. Since the beginning of the twenty-first century, there have been refinements of concepts. The 2010 review of McDonald's criteria allowed the diagnosis of MS with only a proven lesion (CIS). In 1996, the National Society of Multiple Sclerosis (NMSS) of the United States (Clinical Test Advisory Committee) defined the first version of the clinical phenotypes currently used. In this first version they provided standardized definitions for 4 clinical MS courses: relapse-remitting (RR), progressive secondary (SP), progressive primary (PP), and progressive relapse (PR). In 2010, the poverty rate was reduced and CIS was incorporated. Subsequently, three years later, the 2013 review of the "phenotypes for the course of disease" was forced to consider the CIS as one of the phenotypes of the EM, making obsolete some expressions such as "conversion of the CIS to the EM". Other organizations have later proposed new clinical phenotypes, such as HAMS (Highly Active MS) as a result of work in DMT approval processes. Historical Cases[]There are several historical accounts of people who probably had MS and lived before or shortly after the disease was described by Charcot. A young woman named Halldora who lived around 1200 suddenly lost her vision and mobility but, after praying to the saints, she recovered them seven days later. (1380-1433), a, may be one of the first people clearly identifiable with MS. From the age of 16 to her death at 53, she had intermittent pain, leg weakness and vision loss, typical symptoms of the EM. Both cases have led to the proposal of a "gen viking" hypothesis for the spread of the disease. (1794-1848), son of and grandson of , almost certainly had MS. D'Este left a detailed journal describing her 22 years living with the disease. His diary began in 1822 and ended in 1846, although he remained unknown until 1948. His symptoms began at 28 years with sudden temporary visual loss () after a friend's funeral. During his illness, he developed leg weakness, clumsiness of hands, numbness, dizziness, bladder alterations, and . In 1844, he started using a wheelchair. Despite his illness, he maintained an optimistic view of life. Another early MS story was maintained by the British diarist, Bruce Frederick Cummings (1889-1919), who kept a detailed record of his diagnosis and struggle. His journal was published in 1919 as . Research[] This section needs to be updated. Please update this article to reflect recent developments or information recently available. (October 2020)Up-to-date medications[]There is ongoing research in search of more effective, convenient and tolerable treatments for relapse of the EM; creation of therapies for progressive subtypes; strategies; and effective symptomatic treatments. During the years 2000 and 2010, a number of oral medications are expected to be obtained in popularity and frequency of use. Several more oral medications, including , and . Laquinimod was announced in August 2012 and is in a third phase III test after mixed results in the previous ones. Studies are also being conducted to improve the effectiveness and ease of use of existing therapies. This includes the use of new preparations, such as the interferon-β-1a version, which is expected to be given at less frequent doses with similar effects. Striol, a female sex hormone found at high concentrations during late pregnancy, has been identified as a candidate therapy for women with EM relapse and has progressed through phase II tests. Peginterferon beta-1a approval is expected during 2013. Preliminary data suggest that , an anti- , could have benefits in multiple sclerosis. However, the evidence is insufficient to determine the effects as an additional therapy for beta-1a interferon in people with RRMS. high levels of interest have also increased. Since 2012 , , and monoclonal antibodies like , and all had shown some benefit and were being studied as potential treatments, and the FDA approved ocrelizumab for relapse and primary MS in March 2017. Their use has also been accompanied by the emergence of potentially dangerous adverse effects, the most important of which are opportunistic infections. In relation to these research, an antibodies test has been developed, which could help determine who is at the greatest risk of developing progressive multifocal leucoencephalopathy by taking natalizumab. Although monoclonal antibodies will probably have some role in treating the disease in the future, it is believed that it will be small due to the risks associated with them. Another research strategy is to evaluate the two or more drugs. The main reason for using several medications in MS is that the treatments involved point to different mechanisms and therefore their use is not necessarily exclusive. , in which one medicine improves the effect of another are also possible, but there may also be inconveniences such as blocking the action of other side effects or worsened. There have been several trials of combined therapy, however none have shown sufficient positive results to be considered a useful treatment for MS. Research on neuroprotection and regenerative treatments, such as , while of high importance, are in the early stages. There are also no effective treatments for progressive variants of the disease. Many of the most recent drugs, as well as those that are developing, will probably be evaluated as PPMS or SPMS therapy. Medicines that influence sodium ion channels powered by tension are being investigated as a possible neuroprotective strategy due to the hypothesized role of sodium in the pathological process leading to axonal injury and the accumulation of disability. Currently, there is insufficient evidence of a sodium channel blocker effect for people with MS. Pathogenesis[]MS is a clinically defined entity with several atypical presentations. Some auto antibodies have been found in atypical cases of MS, giving birth to families separated from diseases and restricting the previously broader concept of MS. First, they were found in (NMO), which was previously considered a variant of MS. After that, a whole spectrum of diseases called NMOSD (NMO spectrum diseases) or anti-AQP4 have been accepted. Later, it was found that some cases of MS were presenting, mainly superimposed with the . Anti-MOG autoantibodies were also present in ADEM, and a second spectrum of separate diseases is now being considered. At this time, it is called inconsistently through different authors, but it is usually something similar to . Finally, a third type of car antibodies is accepted. They are several autoantibodies that damage the Ranvier nodes of neurons. These antibodies are more related to peripheral nerve demystination, but they were also found in chronic progressive PPMS and (CCPD, which is considered another atypical MS presentation). In addition to all these found autoantibodies, four different patterns of demythation have been reported in MS, opening the door to consider MS as a . Biomarkers of Diseases[] Although the diagnostic criteria are not expected to change in the near future, it is working to develop to help diagnose and predict disease progression. New diagnostic methods that are being investigated include work with anti-myeline antibodies, and studies with serum fluid and cephaloraquíde, but none of them has given reliable positive results. Currently, there are no laboratory research that can predict the prognosis. Several promising approaches have been proposed: , and , , and -A. Since the progression of the disease is the result of neuron degeneration, the roles of proteins that show the loss of nervous tissue like, , and are under investigation. Other effects include looking for biomarkers that distinguish between those who will and will not respond to medicines. Improvement of neuroimaging techniques such as (PET) or (MRI) carries a promise to improve diagnosis and predictions of prognosis, although the effect of such improvements in daily medical practice may take several decades. As for MRI, there are several techniques that have already shown some usefulness in research environments and could be introduced in clinical practice, such as double-investment recovery sequences, , and . These techniques are more specific to the disease than existing ones, but there is still a lack of standardization of acquisition protocols and the creation of policy values. There are other techniques in development that include contrast agents capable of measuring peripheral levels, inflammation or neuronal dysfunction, and techniques that measure the iron deposition that could serve to determine the role of this feature in the EM, or that of brain perfusion. Similarly, the new PET could serve as markers of altered processes such as brain inflammation, cortical pathology, or remyelination. Antibiodies against the potassium channel may be related to MS. Chronic cerebrospinal venous insufficiency[]In 2008, the vascular surgeon suggested that MS involves narrowing of veins that drain the brain, to which it refers (CCSVI). He found CCSVI in all patients with MS in his study, performed a surgical procedure, then called the media the "release procedure" to correct it, and claimed that 73% of the participants improved. This theory received significant attention in the media and among those with MS, especially in Canada. Concerns have been raised with Zamboni's research, as it was not blinded or controlled, and its assumptions about the underlying cause of the disease are not supported by known data. In addition, other studies have not found a similar relationship or found one that is much less strong, raising serious objections to the hypothesis. The "release procedure" has been criticized for resulting in serious complications and deaths with untested benefits. Therefore, since 2013 it is not recommended for the treatment of the EM. Additional investigations are under way to investigate the CCSVI hypothesis. [] 224ab More reading[]12 External links[] Wikimedia Commons has media related to . ################ Research and diagnosis Approved treatment[] Other treatments Demyleinating diseases Other Other Other Diseases of , mainly Cerebro and / and Episodes/ Other Other Both/ya Cerebro and and Episodes/ Other Other and and Other and/() Foreign Autoimmune / Foreign Autoimmune " ()Foreign Autoimmune /() Foreign Autoimmune Unknown/multiple Foreign Autoimmune Foreign Autoimmune Foreign Autoimmune " " Foreign Autoimmune Foreign Autoimmune Foreign Autoimmune Navigation menu Personal tools Named spaces Variants Views More Search Navigation Contributed Tools Printing/exporting Other projects Languages

History of Multiple Sclerosis – MSAA

History of Multiple Sclerosis - YouTube

History of MS | MS Trust

History of Multiple Sclerosis | Visual.ly

Multiple Sclerosis

A Short History of MS | Everyday Health

History of MS (8): Clinical course – Multiple Sclerosis Research Blog

History of Multiple Sclerosis Infographic | Multiple sclerosis, Multiple sclerosis awareness, Disease

Multiple Sclerosis: The History of a Disease: Murray MS, Dr. T. Jock: 9781888799804: Amazon.com: Books

Touched by the Lord's hand: The history of Multiple Sclerosis – Museum of Health Care Blog
The genetics of multiple sclerosis | Practical Neurology
A Brief History of Multiple Sclerosis | MS Strength

Natural history of multiple sclerosis - Neurologic Clinics

Natural History of Multiple Sclerosis: Early Prognostic Factors - Neurologic Clinics
/diagnosis-of-multiple-sclerosis-2440691_final-975f9ab094e64cc69452fb534ed4f981.png)
How Multiple Sclerosis Is Diagnosed

New perspectives in the natural history of multiple sclerosis | Neurology

Multiple sclerosis - ScienceDirect
Multiple sclerosis | Nature Reviews Disease Primers
Multiple Sclerosis
PDF) A History of Multiple Sclerosis Investigations in Canada Between 1850 and 1950
PDF) Natural History of Multiple Sclerosis Symptoms

Multiple sclerosis symptoms - Book chapter - IOPscience
Multiple Sclerosis. What is Multiple Sclerosis? It is an Auto Immune Disease which is when the body starts to destroy itself. It is a life-long disease. - ppt download

Multiple sclerosis | Practical Neurology

The history of multiple sclerosis: the changing frame of the disease over the centuries | Semantic Scholar
Multiple Sclerosis
Multiple sclerosis - Wikipedia
Reaching an evidence-based prognosis for personalized treatment of multiple sclerosis | Nature Reviews Neurology

History of Multiple Sclerosis | Springer Publishing
Multiple sclerosis 2015

Clinical Features and Natural History of Multiple Sclerosis: The Nature of the Beast - ScienceDirect

Treatment of Multiple Sclerosis: A Review - The American Journal of Medicine

PDF) History of multiple sclerosis

Development of an Integrated Multiple Sclerosis Flowsheet Registry to Bridge the Gap between Electronic Health Record Functionality and Clinical Information Needs
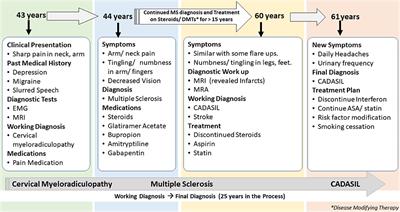
Frontiers | CADASIL vs. Multiple Sclerosis: Is It Misdiagnosis or Concomitant? A Case Series | Neurology

Natural History of Multiple Sclerosis with Childhood Onset | NEJM
Natural history of multiple sclerosis: risk factors and prognostic indicators

The History of Multiple Sclerosis: Part 1 | Multiple sclerosis, Multiple sclerosis awareness, Autoimmune disease awareness

Demyelinating disease in a patient with psoriatic arthritis and family history of multiple sclerosis treated with infliximab. | The Journal of Rheumatology
PDF) The first case history of multiple sclerosis: Augustus d'Est, (1794-1848)
Posting Komentar untuk "history of multiple sclerosis"